What is renal cell carcinoma?
More than 70,000 people in the United States are diagnosed with kidney cancer each year. Renal cell carcinoma (RCC), or renal cell cancer, is the most common type of kidney cancer, accounting for about 90% of all cases. In this type of cancer, malignant cells form in the lining of tubules (very small tubes) of the kidneys.
What causes renal cell carcinoma?
Cancer occurs when abnormal cells begin to grow or divide uncontrollably. The abnormal cells crowd out normal cells, causing problems at the site where the cancer started. Cancer can sometimes spread to other organs as well. RCC beings in one or both kidneys.
The kidneys are bean-shaped organs that filter blood and create urine to dispose of the waste. Renal cell cancer affects the lining of small tubules in the kidneys, where the filtration takes place.
Most people have two kidneys — one on each side of the lower spine, near the hips. However, it’s possible to live a healthy life with just one kidney. RCC usually involves one tumor in one kidney, but it also may involve multiple tumors in both kidneys.
Certain factors and lifestyle choices affect your risk of getting RCC. You may have an increased risk of RCC if you:
smoke
use pain medicines, including over-the-counter medications, for a long period of time
have a family history of RCC or a related genetic condition
are overweight
have high blood pressure
What are the signs and symptoms of renal cell carcinoma?
People with RCC may not experience any symptoms, particularly in the early stages. But you should talk to your doctor if you have:
blood in your urine also called hematuria
a lump in your abdomen or back
pain in your side that doesn’t go away
loss of appetite or unexplained weight loss
anemia (low red blood cell count)
How is renal cell carcinoma diagnosed?
If your doctor suspects you may have renal cell cancer, you will have a series of tests, including:
Physical exam: Your doctor will check for signs of disease, such as a lump near your kidney.
Health history: You will provide a detailed list of any conditions you and your family members have had. Your doctor will also ask about your health habits and lifestyle choices.
Imaging tests: Ultrasound, magnetic resonance imaging (MRI), and computed tomography (CT) scans take detailed pictures of your kidneys and other tissues inside the abdomen.
Blood tests: Your doctor may order tests that measure blood cell counts and kidney function.
Urinalysis: Urine tests check the urine for signs of protein and blood that could indicate cancer or other kidney diseases.
Biopsy: This definitive test for kidney cancer uses a thin needle to remove a bit of tissue. A pathologist (lab specialist) examines the sample for evidence of cancer cells.
What are the types of renal cell carcinoma?
There are several different types of RCC. Your doctor will determine which type you have in order to choose the right treatment for you. The information also may determine whether your relatives could be at risk for a genetic syndrome. The types of RCC are:
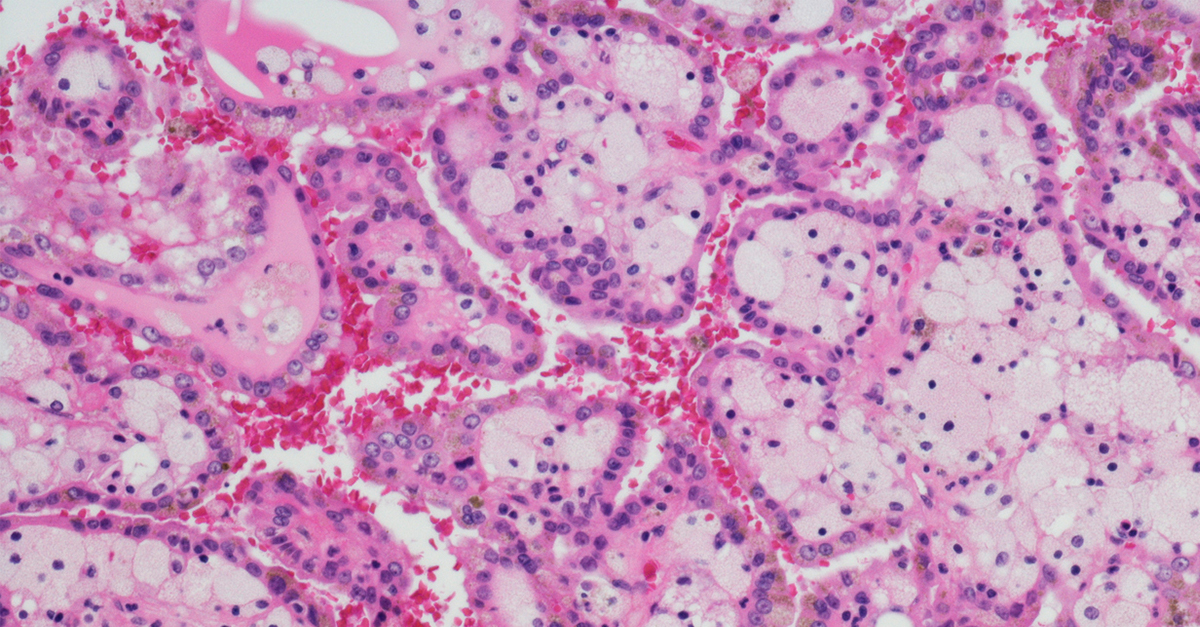
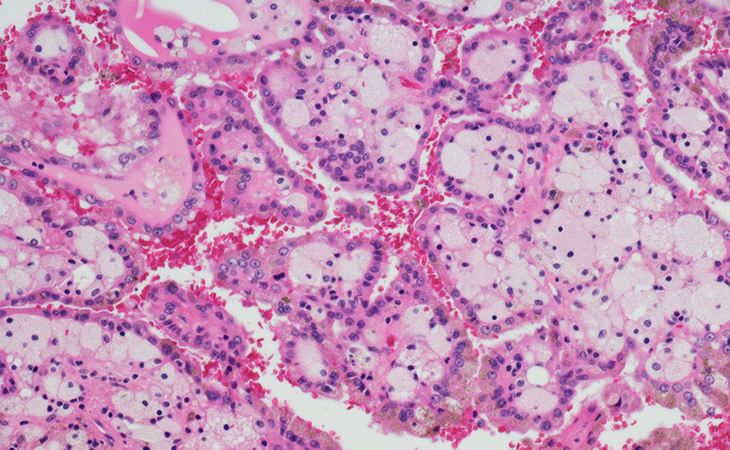
Clear cell RCC
Clear cell RCC is the most common subtype. About 70% of renal cell carcinomas are this type. Under a microscope, cells with clear cell RCC look pale or clear. All other subtypes are classified as non-clear cell RCC.
Papillary renal cell carcinoma
Papillary renal cell carcinoma cells have small finger-like projections (called papillae) that stick out of the tumor. This type is also called chromophilic RCC because the cells easily absorb color from stains. Stains applied to cells in the lab help scientists see cell details and make a diagnosis. About 10% of renal cell carcinomas are this type.
Chromophobe renal cell carcinoma
These cells also appear pale, but they are larger and have thicker borders. Chromophobe renal cell carcinoma accounts for about 5% of RCC.
Rare types of RCC
The remaining cases of RCC make up about 1% of cases. These types include:
collecting duct RCC
multilocular cystic RCC
medullary carcinoma
mucinous tubular and spindle cell carcinoma
neuroblastoma-associated RCC
Sometimes, RCC is unclassified because its appearance does not fit well into any of the categories.
What are the stages of RCC?
Doctors use staging to determine if cancer has spread beyond the kidneys. RCC may spread, or metastasize, to other parts of the body through tissue, the lymph system, or the blood. Doctors determine cancer stage based on tumor size and whether the cancer has spread beyond the kidneys and to other organs.
RCC is staged from I to IV. Stage I means cancer is only in the kidney, and stage IV indicates it has spread (metastasized) to other organs and lymph nodes.
How is renal cell carcinoma treated?
Based on the type and stage of RCC, your doctor will recommend a treatment plan. The plan may include one or more of the following approaches:
Surgery: This is the most common treatment for kidney cancer. Surgery can often cure early-stage RCC.
Radiation therapy: Also called radiotherapy, this treatment uses beams of intense energy to kill cancer cells or stop them from growing.
Thermal ablation: Your doctor inserts a needle into the tumor and applies heat to kill cancer cells.
Cryosurgery: Cold liquid nitrogen is delivered directly to the tumor through a needle kill cancer cells
Immunotherapy: Leading-edge immunotherapy drugs prompt your own immune system to fight the cancer.
Targeted therapy: These medications attack specific parts of cancer cells to stop them from growing and multiplying.
Chemotherapy: Oral or intravenous medications stop cancer cells from growing.
What is the outlook for people with renal cell carcinoma?
The earlier RCC is detected, the better. Overall, about 75% of people with kidney cancer are alive five years after their diagnosis. When cancer hasn’t spread beyond the kidney, survival rates are high as 93%.
Even if your treatment is successful, RCC can come back. This is called recurrence. It’s important to have a follow-up plan with your doctor after treatment for RCC to detect a recurrence as soon as possible.
From the community: “I have metastatic renal cell cancer--first diagnosed December, 2008--which has been well treated with multiple surgeries (including a total pancreatectomy 5 yrs ago) and multiple systemic treatments over the years--you name it, I've probably had it! So don't lose hope. There have been 2 or 3 dark periods for me over the past 11 years, when I thought “this is it, the end”, but some new treatment or clinical trial or surgery has always come up that either removed or reduced my tumors or at the very least stabilized their growth for a year or more, giving me time until the next “best treatment” appeared on the horizon. I'm now age 70, doing well, physically quite active and enjoying my recent retirement. For all practical purposes, my renal cell cancer has become a chronic disease and there’s a reasonable chance I'll ultimately beat this.” - Inspire member
Sources
About Kidney Cancer. American Cancer Society. February 2020.
Survival Rates for Kidney Cancer. American Cancer Society. February 2020.
What’s New in Kidney Cancer Research? American Cancer Society. February 2020.
Kidney Cancer: Types of Treatment. American Society of Clinical Oncology. August 2019.
Gale Harding G, et al. Symptom burden among patients with renal cell carcinoma (RCC): content for a symptom index. Health and Quality of Life Outcomes. June 2007.
Cancer Stat Facts: Kidney and Renal Pelvis Cancer. National Cancer Institute.
Clear Cell Renal Cell Carcinoma. National Cancer Institute. March 2020.
Genetics of Kidney Cancer (Renal Cell Cancer) (PDQ®) – Health Professional Version. National Cancer Institute. May 2020.
Renal Cell Cancer Treatment (PDQ®) – Patient Version. National Cancer Institute. July 2020.
What Is Kidney Cancer? Urology Care Foundation.
Disclaimer
Member comments are lightly edited for length and to remove identifying information but are otherwise reproduced as they appear in the community as part of public posts.
This content is for general informational purposes only and does not necessarily reflect the views and opinions of any organization or individual. The content should not be used as a substitute for professional medical advice, diagnosis, or treatment. Please consult your healthcare provider about any questions you may have regarding a medical condition.




